What is Diabetic Retinopathy?
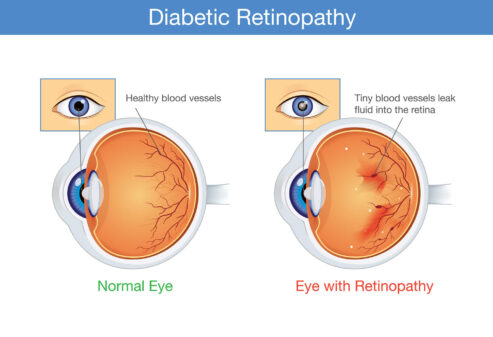
Diabetic Retinopathy is a complication of diabetes that affects the retina, the light-sensitive layer of tissue at the back of the eye. It can cause vision loss and blindness and result from damage to the retina’s blood vessels from high blood sugar levels associated with uncontrolled diabetes.
There are two main types of diabetic retinopathy:
- Non-proliferative diabetic retinopathy (NPDR) is the most common form of diabetic eye disease and is usually symptomless. It is characterized by small bulges called microaneurysms on the retina, which can cause vision changes. This stage of diabetic retinopathy can lead to severe complications if left untreated, so it’s essential to monitor for symptoms and seek treatment if necessary regularly.
- Proliferative diabetic retinopathy (PDR) is the advanced stage of the disease, characterized by the growth of new blood vessels on the retina and, in the vitreous, the clear gel that fills the interior of the eye. These new blood vessels are fragile and prone to bleeding, which can cause vision loss and severe vision impairment. In addition, scar tissue can form on the retina and pull it away from its normal position, leading to retinal detachment.
What are the 4 stages of diabetic retinopathy?
Diabetic retinopathy is a progressive disease that typically goes through four stages:
- Mild Non-proliferative Retinopathy (Early stage): mild symptoms are present, characterized by microaneurysms and small abnormalities in blood vessels. At this point, no significant symptoms or vision loss is typically experienced.
- Moderate Non-proliferative Retinopathy (Intermediate stage) is characterized by the blockage of some of the smaller blood vessels in the retina, which can cause vision changes.
- Severe Non-proliferative Retinopathy (Advanced stage) is characterized by the blockage of many of the smaller blood vessels in the retina, leading to ischemia (a lack of blood flow to the retina). This stage can cause vision changes and is a warning sign of proliferative diabetic retinopathy.
- Proliferative Diabetic Retinopathy (PDR) (Advanced stage) occurs and is marked by the development of new blood vessels in the retina and vitreous, which is the clear gel that fills the interior of the eye. These delicate blood vessels tend to bleed, leading to potential vision loss and severe visual impairment.
People with diabetes must undergo regular eye exams, as early detection and treatment can help prevent the progression of diabetic retinopathy and preserve vision.
What Causes Diabetic Retinopathy?
Diabetic Retinopathy is caused by long-term elevated blood sugar levels associated with uncontrolled diabetes. Over time, high blood sugar levels can damage the tiny blood vessels in the retina, leading to a range of changes and complications in the tissue.
Initially, small blood vessels in the retina may become leaky, causing swelling in the surrounding tissue and blurring vision. As the disease progresses, the blood vessels may close off completely, cutting off the blood supply to the retina and causing the formation of new, abnormal blood vessels that can easily bleed and further damage the retina.
If left untreated, diabetic retinopathy can cause vision loss, including blindness. Early detection and proper control of blood sugar levels, as well as prompt treatment, can help slow or prevent the progression of diabetic retinopathy.
Who is at Risk for Developing Diabetic Retinopathy?
Anyone with diabetes is at risk for developing diabetic retinopathy. Still, the risk is more significant for people with the disease for a long time and those with poorly controlled blood sugar levels. Other risk factors for diabetic retinopathy include:
- High blood pressure
- High cholesterol levels
- Pregnancy
- Kidney disease
- Smoking
Individuals with diabetes need to have regular comprehensive eye exams to detect diabetic retinopathy in its early stages and to receive prompt treatment to help prevent vision loss.
Symptoms of Diabetic Retinopathy.
In its early stages, diabetic retinopathy may not cause any noticeable symptoms. However, as the disease progresses, some of the following symptoms may develop:
- Blurred vision
- Fluctuating vision
- Shadows or missing areas of vision
- Double vision
- Dark or floating spots in the vision
- Difficulty with bright lights
- A need for more light when reading or doing close work
- Reduced color vision
- A sudden loss of vision in one eye
It is important to have regular comprehensive eye exams to detect diabetic retinopathy in its early stages if you have diabetes, even if you do not have any symptoms so that prompt treatment can be given to help prevent vision loss.
Risk Factors for Diabetic Retinopathy
The following factors may increase the risk of developing diabetic retinopathy:
- Duration of diabetes: People with diabetes are more likely to experience diabetic retinopathy the longer they have had the condition. The duration of diabetes can have a significant impact on the severity and onset of this ocular disease.
- Poorly controlled blood sugar levels: High blood sugar levels over a prolonged period can damage the blood vessels in the retina.
- High blood pressure: Elevated blood pressure can damage blood vessels and increase the risk of diabetic retinopathy.
- High cholesterol levels: High cholesterol levels can increase the risk of cardiovascular disease and other diabetic complications, including diabetic retinopathy.
- Pregnancy: Women with diabetes who are pregnant have an increased risk of developing diabetic retinopathy.
- Kidney disease can increase the risk of diabetic retinopathy and other diabetic complications.
- Smoking increases your risk of diabetic retinopathy and other related health issues associated with diabetes.
Individuals with diabetes need to have regular comprehensive eye exams to detect diabetic retinopathy in its early stages and to receive prompt treatment to help prevent vision loss.
Treatments for Diabetic Retinopathy
Treatments for diabetic retinopathy can be divided into two categories, depending on the stage of the disease: early diabetic retinopathy and advanced diabetic retinopathy.
Early diabetic retinopathy treatments include:
- Tight control of blood sugar, blood pressure, and cholesterol levels through diet, exercise, and medications
- Laser therapy to prevent or slow the progression of retinal damage
Advanced diabetic retinopathy treatments include:
- Intravitreal injections of anti-VEGF drugs slow the growth of new blood vessels and reduce the risk of bleeding.
- Laser therapy to seal leaking blood vessels and prevent further vision loss
- Surgical procedures, such as vitrectomy or implantation of a device to drain fluid from the eye, to treat more severe cases
You must have regular eye exams to monitor the progression of diabetic retinopathy and initiate appropriate treatment early on.
Complications of Diabetic Retinopathy
Diabetic retinopathy can lead to several serious complications, including:
- Vision loss or blindness: damage to the retina caused by leaking blood vessels or retinal detachment.
- Macular edema is a medical condition that affects the macula, a part of the retina responsible for sharp, detailed vision. Swollen can cause vision impairment and even blindness if left untreated.
- Vitreous hemorrhage is a condition characterized by bleeding within the vitreous, the jelly-like substance that fills the back region of the eye. This can cause floaters and a decrease in vision.
- Retinal detachment occurs when the delicate retina at the back of the eye becomes separated from its normal position on the inner surface of the eyeball. This can cause vision loss and will require immediate medical attention.
- Glaucoma is a vision-related eye condition that occurs when the internal pressure inside the eye elevates too high, causing damage to the optic nerve and potentially resulting in vision loss or blindness.
- Cataracts occur when the eye’s lens becomes cloudy or opaque, decreasing vision quality. Cataracts can range from mild to severe and can cause problems with color perception, glare sensitivity, and blurriness.
It is vital for people with diabetes to undergo regular eye exams and to manage their blood sugar levels to help prevent the development and progression of diabetic retinopathy and its complications.
Prevention and Management Tips for Diabetes Patients.
Here are some tips for preventing and managing diabetes:
- Eating a healthy diet: Focus on eating fresh fruits, vegetables, whole grains, lean protein, and healthy fats.
- Exercising regularly: To maintain good health, it is essential to make exercising part of your daily routine. Aim for 30 minutes or more of moderate physical activity daily, such as walking or cycling at a brisk pace.
- Maintaining a healthy weight: Maintaining a healthy weight through diet and exercise can help prevent and manage diabetes.
- Monitoring blood sugar levels: Regular monitoring of blood sugar levels is vital for managing diabetes and avoiding complications.
- Taking medications as prescribed: If prescribed, take your medications and insulin as directed.
- Quitting smoking is essential for diabetes prevention and management. Smoking can contribute to the risk of developing diabetes, and quitting smoking can help lessen or even prevent this risk. Additionally, it can improve the overall health of people who already have diabetes.
- Reducing stress: Chronic stress can affect blood sugar levels, so finding ways to manage stress is vital for managing diabetes.
- Regular exams: Getting regular check-ups is an essential part of managing diabetes. Seeing your healthcare provider regularly can help monitor blood glucose levels, detect and prevent complications, and effectively manage the disease.
It’s important to remember that everyone’s experience with diabetes is unique, and working closely with a healthcare provider can help you create a personalized plan for managing the disease.
When to See an Eye Doctor
People with diabetes should see an ophthalmologist or optometrist at least once a year or more often if their doctor recommends it.
In addition, people with diabetes should seek immediate medical attention if they experience any sudden changes in their vision, such as blurred vision, floaters, flashes of light, or a sudden loss of vision. These symptoms may indicate the development of diabetic retinopathy or another eye condition that requires prompt treatment to prevent vision loss.
Regular eye exams and adequate treatment can help prevent the progression of diabetic retinopathy and preserve vision.
Summary
Diabetic retinopathy is a common complication of diabetes that can lead to vision loss and blindness if left untreated. It is caused by damage to the blood vessels in the retina and is classified into two main stages: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). NPDR is the early stage of the disease, while PDR is the advanced stage, characterized by the growth of new blood vessels in the eye.
People with diabetes should undergo regular eye exams and manage their blood sugar levels to help prevent the progression of diabetic retinopathy and its complications.
Early detection and treatment can help preserve vision. If you experience sudden changes in your vision, seek immediate medical attention.






