Introduction
What Is Open-Angle Glaucoma?
How Common Is It?
- Open-angle glaucoma affects more than 70 million people worldwide. It is the leading cause of irreversible blindness.
- The risk of open-angle glaucoma increases after age 40. Up to 10% of people over age 70 are affected.
- People with a family history of glaucoma, those of African or Hispanic descent, and people with high eye pressure are at higher risk.
Causes and Risk Factors
The exact cause of open-angle glaucoma is not fully understood, but several factors can increase the risk:
1. Increased Intraocular Pressure (IOP)
2. Age
Open-angle glaucoma is most common after age 40. The risk doubles with each decade after age 60.
3. Genetics and Family History
Having a parent or sibling with glaucoma increases the risk by up to nine times.
4. Race and Ethnicity
- Open-angle glaucoma is more common and often more aggressive in people of African descent.
- It also tends to develop at a younger age in Hispanic populations.
5. Systemic Diseases
- Diabetes
- High blood pressure
- Sleep apnea
6. Long-Term Corticosteroid Use
Steroid eye drops or oral medications can increase eye pressure over time.
7. Thin Cornea or High Myopia
Certain structural features of the eye, such as a thin cornea or severe nearsightedness, can increase the likelihood of optic nerve damage.
Symptoms of Open-Angle Glaucoma
By the time symptoms appear, the optic nerve is often already damaged.
- Gradual loss of peripheral (side) vision
- Difficulty seeing in dim light
- Needing more light to read
- Blurred vision in later stages
- Tunnel vision (advanced disease)
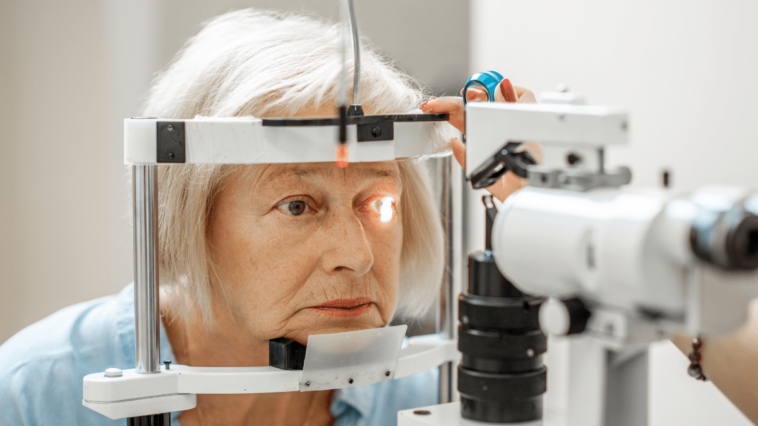
How Open-Angle Glaucoma Is Diagnosed
1. Intraocular Pressure Measurement (Tonometry)
Determines if the pressure inside the eye is above normal (typically > 21 mmHg).
2. Optic Nerve Evaluation (Ophthalmoscopy)
The doctor examines the optic disc for signs of cupping or thinning of the optic nerve.
3. Visual Field Test (Perimetry)
Maps the patient’s side vision to detect early defects.
4. Optical Coherence Tomography (OCT)
Provides detailed images of the retinal nerve fiber layer to monitor progression.
5. Gonioscopy
People at higher risk, such as those with a close family member with glaucoma, people of African or Hispanic descent, or those with high eye pressure or diabetes, should start screening before age 40 and have exams every year or as recommended by their eye doctor.
Early and regular screening helps find glaucoma when it is easier to treat.
Treatment: Controlling the Pressure to Protect Vision
The main goal of treatment is to lower eye pressure to a safe level and prevent further damage to the optic nerve.
Glaucoma cannot be cured, but with the right treatment and regular follow-up, its progression can be slowed or stopped.
1. Eye Drops (First-Line Therapy)
- Prostaglandin analogs (latanoprost, travoprost)
- Beta-blockers (timolol)
- Alpha agonists (brimonidine)
- Carbonic anhydrase inhibitors (dorzolamide)
Most people start treatment with eye drops. It is important to use them exactly as prescribed. Common side effects include redness, stinging, or discomfort. If you notice any side effects or have concerns, talk to your doctor so your treatment can be adjusted if needed.
2. Laser Treatment (Selective Laser Trabeculoplasty – SLT)
- Laser treatment usually lowers eye pressure by 20 to 30 percent.
- It can be used instead of eye drops or together with them.
3. Surgical Treatments
If medications and laser treatments do not lower eye pressure enough, surgery may be needed.
• Trabeculectomy
Creates a new drainage pathway for fluid to exit the eye.
• Tube Shunt Surgery
• Minimally Invasive Glaucoma Surgery (MIGS)
Living with Glaucoma
- Apply eye drops daily as prescribed.
- Attend regular checkups for pressure and visual field tests.
- Monitor side effects or changes in vision.
- Inform doctors about all medications, especially steroids.
Vision changes can affect driving, work, and other daily activities, so it is important to be prepared and talk to your doctor about any concerns.
Can Open-Angle Glaucoma Be Prevented?
- Having regular eye exams after age 40
- Protecting your eyes from injury.
- Keeping your blood pressure and blood sugar at healthy levels.
- Avoiding long-term or excessive use of steroid medications.
- Encouraging your family members to get screened for glaucoma.
Key Takeaways
- Open-angle glaucoma is the most common type of glaucoma and often has no symptoms at first.
- It causes vision loss that gets worse over time and cannot be reversed. It usually starts with loss of side vision.
- Early detection through regular exams is crucial.
- Treatment focuses on lowering eye pressure with drops, laser therapy, or surgery.
- With regular care, most people with glaucoma can keep useful vision for life.
Frequently Asked Questions (FAQ)
1. Is open-angle glaucoma curable?
No. Damage to the optic nerve cannot be reversed, but early and ongoing treatment can help control the disease and slow its progression.
2. Does glaucoma always cause high eye pressure?
Most cases of glaucoma involve high eye pressure, but some people develop glaucoma even when their eye pressure is normal. This is called normal-tension glaucoma.
3. Can I use my drops irregularly?
No. Skipping doses can cause your eye pressure to rise and may speed up vision loss.
4. Is laser treatment permanent?
SLT can work for several years and can be repeated safely if your eye pressure goes up again.
Yes. Regular exercise, eating a healthy diet, and avoiding smoking or stress can help support your eye health.
References
- American Academy of Ophthalmology (AAO). Primary Open-Angle Glaucoma Preferred Practice Pattern®, 2023.
- National Eye Institute (NEI). Facts About Glaucoma.
- European Glaucoma Society (EGS). Guidelines on Glaucoma Management, 2021.
- World Health Organization (WHO). Vision 2020: The Right to Sight – Global Initiative for the Elimination of Avoidable Blindness.
- Weinreb RN, et al. The Pathophysiology and Treatment of Glaucoma: A Review. JAMA, 2014.